Connect with providers
at the point-of-care
Retrace is the easiest, fast way to create two way data links between payers and providers at the point of care. Using payer and employer data to enhance existing EHR interfaces, Retrace enables providers to improve healthcare outcomes, quality, cost and member satisfaction.

Instant results without limits
We handle the confusion of navigating multiple disjointed platforms and systems by seamlessly connecting providers, patients, and payers with our end-to-end platform.

Retrace Connect

Retrace Optics
Retrace Connect
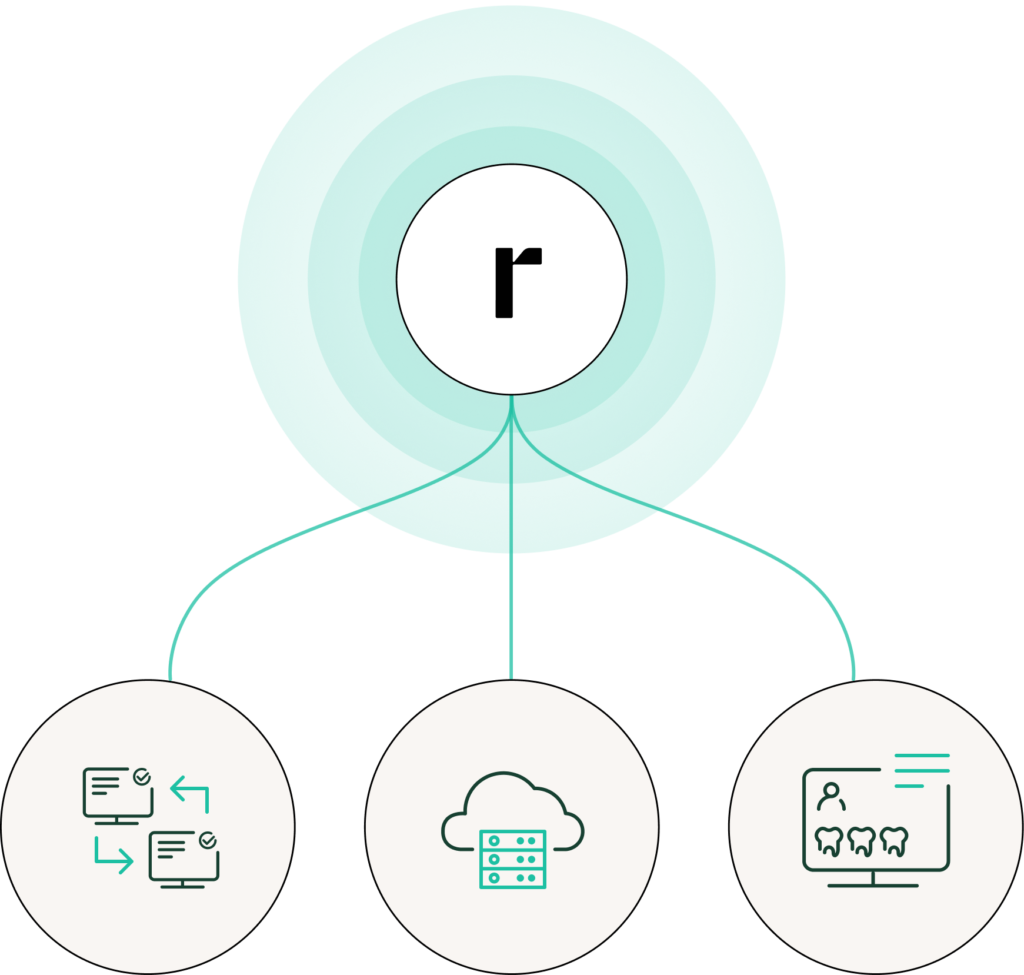
How Retrace Powers Healthcare Networks
- Increased practice productivity
- Predictable and accurate quality care guidance
- Integrated systems that work alongside point-of-care
Engage Beyond Payments
Empower your network to resolve their bills

Retrace Connect Features
Pioneering painless payments for payers, providers, and
patients

Why Leaders Choose Retrace Connect
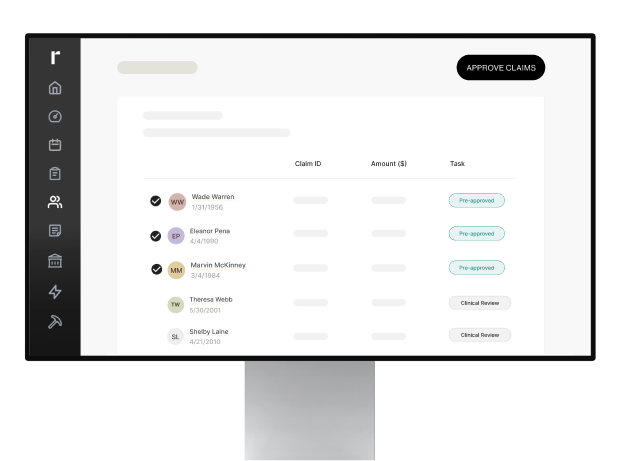
Instant, automated claim payment
Give members and providers
the most frictionless healthcare
payment experience
Tech that evolves without interruption
Use the cloud-based solution that’s
always learning and improving
Help members help themselves
Enable members to quickly
and easily resolve common
claim and billing issues
Real-time Insights with Retrace Optics
Robust analytics, data driven decision-making
Retrace Optics Features
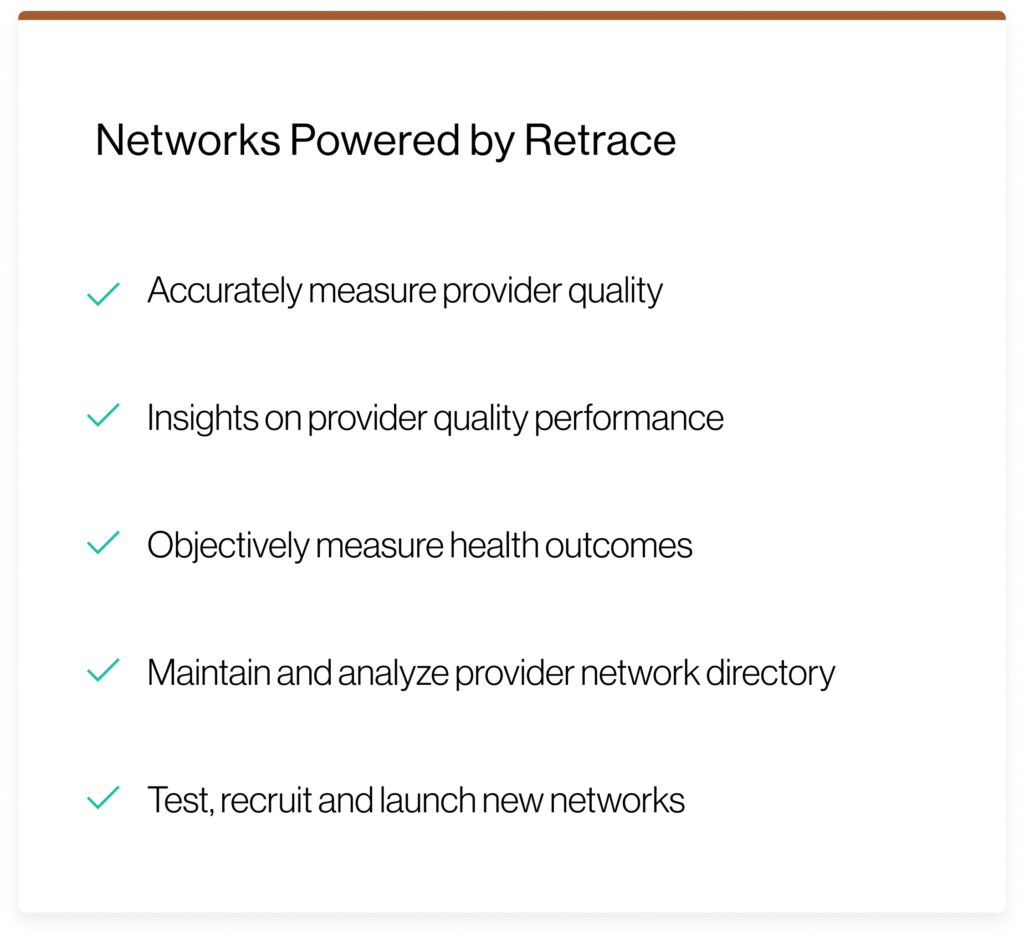
How payers use Retrace
With Retrace Optics, payers reduce costs and improve the
experiences of their members, providers, and partners.


Provider
Directories
Provider
Networks

Provider
credentialing
Provider
onboarding

Plan
Performance
Intelligent
engagement
Reliable implementations
Retrace’s proven implementation strategy minimizes disruption and time to value for our partners. Integration is full service, streamlined and fully compatible with all legacy and modern systems.
Predictable Results
30
Day timeframe for implementation
from setup to production
99%
8x
*Based on the source provided